Arlene Shaulis Can Finally Breathe Easy Thanks to Endobronchial Valve Treatment

When Arlene Shaulis was diagnosed with emphysema nearly a decade ago, she had no idea her life would gradually shift into one she didn’t recognize. Getting ready for work and into the office would deplete her energy for the entire day. Her husband would assume most of the household responsibilities. Arlene would spend her weekends recuperating on the couch, exhausted from the work week, instead of out enjoying the life she once knew.
As the severity of Arlene’s symptoms grew, she persisted at work because, she says, “I knew it was the best thing for me.” But the year leading up to her procedure was almost unbearable, and she doesn’t know how she pushed herself to continue. Even worse, Arlene suffered in silence. She was embarrassed by her condition, which was caused by smoking.
Arlene got a second lease on life, thanks to minimally invasive bronchoscopic lung volume reduction (BLVR) that she calls a “medical miracle.” Her procedure was on a Monday. By Thursday she was home, just in time to celebrate her 44th wedding anniversary. Exactly one week after her procedure, she returned to work.
Today, Arlene takes a shower, puts on her makeup, gets dressed for work – and only remembers to take her medicine because of her trusty phone alarm. Before BLVR, she was dependent on albuterol and continuous rounds of prednisone and antibiotics just to survive these basic activities. “My whole life revolved around how I was breathing. Every single minute I was thinking, ‘Can I do this?'”
Arlene’s pulmonologist, James Lamberti, MD, told her about a revolutionary treatment for advanced emphysema. The FDA had fast-tracked the use of endobronchial valves, placed minimally invasively in the lungs, to help patients breathe easier. The valves allow one lobe of the lung to deflate, releasing trapped air, so healthier parts of the lung can take in more air. Patients treated in clinical trials reported immediate relief.
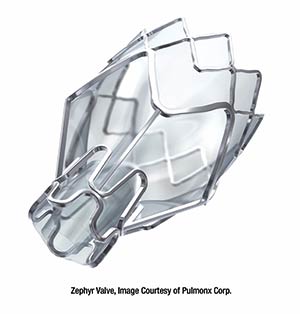
Inova Fairfax Medical Campus (IFMC) is one of the few institutions in the region performing BLVR. The IFMC Interventional Pulmonology Department uses two types of endobronchial valves: the Zephyr® Endobronchial Valve and the Spiration® Valve System. Both reduce lung hyperinflation, the main cause of increased shortness of breath in emphysema patients. The interventional pulmonology team decides which valve is best for each patient based on testing and evaluation. Among other criteria, patients must be nonsmokers for at least four months to be eligible for evaluation.
Arlene received five Zephyr valves in her right lung, which she says was destroyed from smoking. “When I woke up in recovery, I could already feel the difference,” she says. “I still can’t believe it. I feel so blessed that I had this procedure. It’s just incredible.” Arlene is grateful to everyone at Inova – from her interventional pulmonologist, Amit Mahajan, MD (or “Dr. Bobby,” as she calls him), to the lung navigator who coordinated her care, to each nurse, technician and food service team member she encountered. “Inova made it so easy for me. It was like they held my hand,” she says. What does Arlene most want anyone considering endobronchial valve treatment to know? “If you meet the criteria for the procedure, don’t hesitate to do it. And, be very thankful.
Learn More
Learn more about Inova’s BLVR procedure and endobronchial valves, or contact the Inova Lung Services patient navigator at 703-776-4712.
Meet Dr. Amit Mahajan
Dr. Mahajan, Medical Director of Interventional Pulmonology at Inova Fairfax Medical Campus, specializes in BLVR. Learn more about Dr. Mahajan